The company has been around for more than 15 years but only attained the status of a major health care management organization in the last four years, following a merger with a medical management group and an uplisting from the Over-the-Counter Pink Sheets to the Nasdaq.
Apollo Medical already manages 14 physician groups comprised of more than 7,000 physicians providing care to more than 1.1 million patients.
Now the company is taking the next step: It’s going national.
To this point, almost all of Apollo Medical’s clientele and covered patients have been in Southern California. But in January, the company assumed a stake and arranged a strategic alliance with New York-based CAIPA MSO, a management services organization for more than 1,000 physician practices serving more than 500,000 patients in the New York metro area.
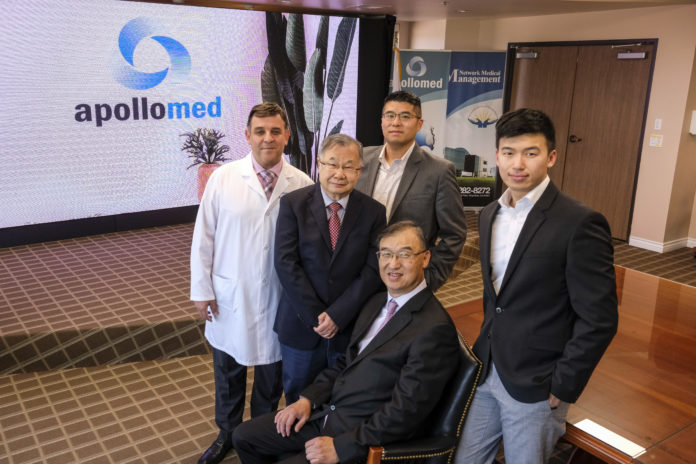
“We have made our first foray outside of California by acquiring a stake in a large physician group in New York City,” said Brandon Sim, Apollo Medical’s chief operating officer and chief technology officer. “It represents a scaling of our model outside of Southern California.”
Shareholders have responded with enthusiasm to this and other recent moves by Apollo Medical, sending shares up 89% over the past 12 months to close at $28.71 on April 28.
The company’s platform manages claims and acts as a gatekeeper for patient treatment. The technology also provides human resources and information technology services and a host of other functions for independent physician associations, or IPAs.
On behalf of these IPAs, which are consolidated groups of hundreds of physician practices, Apollo Medical handles the bulk of interactions with health care insurers. In most cases, this includes managing the contracts between insurers and IPAs.
In today’s capitated cost world — think health maintenance organizations, or HMOs — Apollo Medical manages contract dollars from insurers, making sure that patient treatment plans crafted by physicians within the IPA do not exceed the fixed contract amount. Apollo Medical makes money if actual claims costs are less than the fixed contract amount.
“If we manage the care properly over time, we make money if we disburse less than the fixed contract amount to the (health care) provider,” Sim said.
Extensive experience
Extensive experience
“Technology has expanded our reach and made it easier to achieve the savings and improve the medical outcomes that helps bring in the revenue,” said David Schmidt, a member of Apollo Medical’s board. “A big piece of this is improving the care to reduce future outlay: That’s fewer and shorter hospital stays and fewer ER visits.”
For example, COO Sim said, if Apollo Medical’s software detects that repeated late diagnoses of breast cancer among an IPA’s patient pool is creating higher costs, it can recommend more focus on regular mammogram screening.
Another area of concentration for Apollo Medical is improving efficiency. One local doctor using the company’s system through the IPA he belongs to pointed to rapid turnaround times for approvals for screening procedures.
“If I have to get approval for a patient to have a mammogram or a colonoscopy, I can get an approval quickly through the Apollo Medical portal,” said Paul Liu, an internal medicine and geriatrics solo practitioner in San Marino. “Often, the approval comes through even before I finish typing the request into the system. That helps me a lot, and it especially helps the patient a lot.”
Liu, who has been using Apollo Medical and its predecessor company’s case management software for more than 15 years, said he has been pleased with the general lack of red tape.
Even when a request for treatment might initially be denied, Liu said he has been able to call up medical case managers at Apollo Medical and almost always gets the approval.
“If I had to do this without Apollo Medical — essentially deal directly with the insurer — I probably would have to hire one or two more people just to deal with the requests for treatment and claims management,” he said. “They have been really good at handling this back-office side of things.”
Apollo Medical is one of dozens of medical management companies trying to lower costs and improve patient outcomes for physician groups. It’s a market that has expanded in recent years with the widespread adoption of technology platforms that allow for more data analysis, according to board member Schmidt.
Competitive market
Competitive market
“Apollo’s biggest comparative advantage is the longstanding relationships that its providers have with the patients that they serve,” said Gene Mannheimer, senior research analyst for digital health, information technology and services with Colliers Securities, a unit of Toronto-based Colliers International. “They truly know the patient and, in this manner, can interpret results and make recommendations on care.”
But this in-depth knowledge of patients does pose a challenge, especially as Apollo Medical seeks to expand, he said.
Apollo has set a goal for the rest of this year of nearly doubling the number of patients its participating doctors serve to 2 million from 1.1 million.
Co-Chief Executive Kenneth Sim (father of COO Brandon Sim) said the company is looking to grow organically by signing management contracts with physician groups in other parts of the country and through deals with other medical management companies.
Analyst Mannheimer called the 2 million patient goal “aggressive.”
“In order to build upon the success it has seen through its longstanding relationships at the regional level, Apollo Medical must expand very deliberately and methodically, ensuring that it can replicate its model in geographies outside of Southern California,” he said. “If they acquire too aggressively or indiscriminately, they risk going too far afield from their comfort zone, which could have negative ramifications.”
In this context, Mannheimer said Apollo’s initial move — acquiring a stake in CAIPA MSO — is an appropriate “baby step.”
“Apollo is not taking on lives (patients) in this deal with CAIPA,” he said, adding that if the deal goes well, “it’s reasonable that Apollo may expand the scope of its agreement with CAIPA.”